Diverse sexual orientation, gender identity and sex characteristics are all included in the LGBTQIA+ acronym. A Standard for Sex, Gender, Variations of Sex Characteristics and Sexual Orientation Variables has been produced by the Australian Bureau of Statistics (ABS) in 2020 and provides a useful starting point of terms for clinicians to gain an understanding of the appropriate terminology.
The Victorian Government LGBTQIA+ Inclusive Language Guide expands on the above definitions, detailing this in the table on the right:

Teaching LGBTQIA+ inclusive healthcare provides confidence and competence in your registrar’s ability to deliver appropriate care. A GP or practice nurse may be the first person someone talks to about their emerging diverse sexual orientation or gender identity, and this could happen at any age. Having a health professional who affirms their identity can be very therapeutic.
There are two major reasons for making the effort to know about an individual patient’s LGBTQIA+ status in clinical practice:
LGBTQIA+ inclusive care requires a whole of practice approach, so that the person’s journey through the clinic is safe. Encouraging disclosure of LGBTQIA+ identities starts at the front door, as they need to feel they will be acknowledged and supported. This is particularly important for LGBTQIA+ patients who may have experienced negative attitudes from healthcare providers in the past.
In helping to create an inclusive environment, there are a range of readily available Australian tools to assist. One example is the Rainbow Tick, an accreditation program and framework for planning and implementing organisational change to facilitate LGBTQIA+ inclusive services. Another is the Pride in Health online benchmarking. Intersex community organisations offer the ‘Yellow Tick’ to improve understanding of the health needs of people with intersex variations.

Children can become part of LGBTQIA+ families using multiple strategies, including assisted reproductive technologies, surrogacy, adoption, fostering, co-parenting, being a known sperm or egg donor and sexual intercourse
Further information on contraception, fertility, and pregnancy as part of LGBTQIA+ inclusive healthcare can be found in the GPSA Guide, free to download here.
![]()
The roles the GP can play in LBQ contraception, fertility, and pregnancy:
Registrars should be comfortable asking questions related to sexual behaviour in a safe and appropriate manner. For patients who are trans and gender diverse, and when asking about the gender of partners, using the terms “assigned male at birth” or “assigned female at birth” can be a useful way of asking about sexual practices and knowing the relevant anatomy while respecting the gender identity of all concerned.
Further information on sexual health as part of LGBTQIA+ inclusive healthcare can be found in the GPSA Guide, free to download here.
Advice about safer sex is important. For some people, exploring their new sexual identities can involve unfamiliar sexual behaviour and this could expose them to new STI risks. If this is happening with your patient, it may be important to sensitively discuss risk and to offer regular STI testing.
PrEP should be actively offered to men who have sex with men, trans and gender diverse people, and people who inject drugs who are at risk of HIV transmission. Similarly, PrEP can be commenced at patient request or if there is potential risk of HIV exposure in the future. As of 2021, PrEP is on the general PBS schedule and can be prescribed by any general practitioner.
Further information on STIs as part of LGBTQIA+ inclusive healthcare can be found in the GPSA Guide, free to download here.
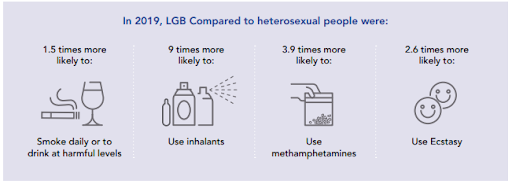
Further information on smoking, alcohol, and drug use as part of LGBTQIA+ inclusive healthcare can be found in the GPSA Guide, free to download here.

Men who have sex with men (MSM) and transgender people may be at risk of ano-rectal Human Papilloma Virus (HPV) infection through anal sex. This is the same type of virus that causes cervical cancer. Further information on cancer screening as part of LGBTQIA+ inclusive healthcare can be found in the GPSA Guide, free to download here.

Date reviewed: 07 April 2024

GPTA Ltd t/as GP Supervision Australia
PO Box 787 Gisborne Vic 3437
Level 40/140 William Street Melbourne Vic 3000